
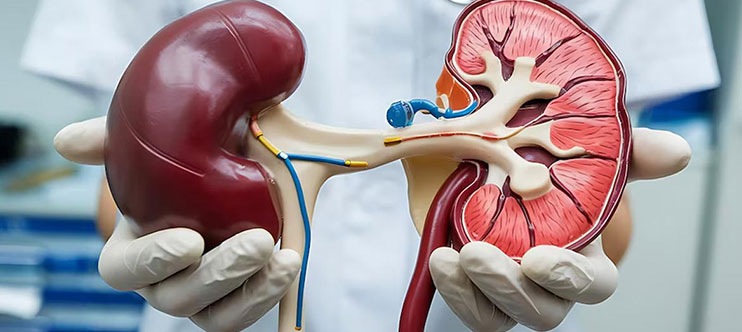
Renal Transplant, also known as Kidney Transplant, is a surgical procedure where a healthy kidney from a donor is transplanted into a patient with end-stage renal disease (ESRD) or chronic kidney failure. The transplanted kidney takes over the function of filtering waste, excess fluid, and toxins from the blood, which the patient’s kidneys can no longer perform effectively.
Indications for Renal Transplant
- End-Stage Renal Disease (ESRD): Irreversible kidney failure requiring dialysis or transplant.
- Chronic Kidney Disease (CKD): Severe decline in kidney function (GFR < 15 mL/min).
- Diabetes and Hypertension: Leading causes of kidney failure.
- Polycystic Kidney Disease: Genetic condition causing enlarged cystic kidneys.
- Glomerulonephritis: Inflammation and damage to the kidney’s filtering units.
How is Renal Transplant Performed?
- Preoperative Evaluation: Imaging , Crossmatch Testing and Blood Tests
- Connection: he renal artery and vein of the donor kidney are connected to the recipient’s iliac artery and vein.
- Incision: A lower abdominal incision is made to place the donor kidney.
Types of Donors
- Living Donor:A family member, friend, or unrelated donor donates one of their kidneys.
- Deceased Donor:A kidney from a brain-dead donor is used for transplantation.
Complications and Risks
- Rejection: The immune system attacks the transplanted kidney.
- Infection: Due to immunosuppression.
- Blood Clots or Bleeding: Post-operative complications.
- Recurrence of Original Disease: May affect the transplanted kidney.
Benefits of Renal Transplant
- Improved Quality of Life
- Restored Kidney Function
- Better Nutrition and Energy Levels
Renal Transplant is the most effective treatment for end-stage renal disease (ESRD), offering a significantly improved quality of life and longer survival. While it requires lifelong monitoring and immunosuppressive therapy, the procedure enables patients to regain normal kidney function and live a healthier, dialysis-free life.